Southwest Center’s Mpox Updates
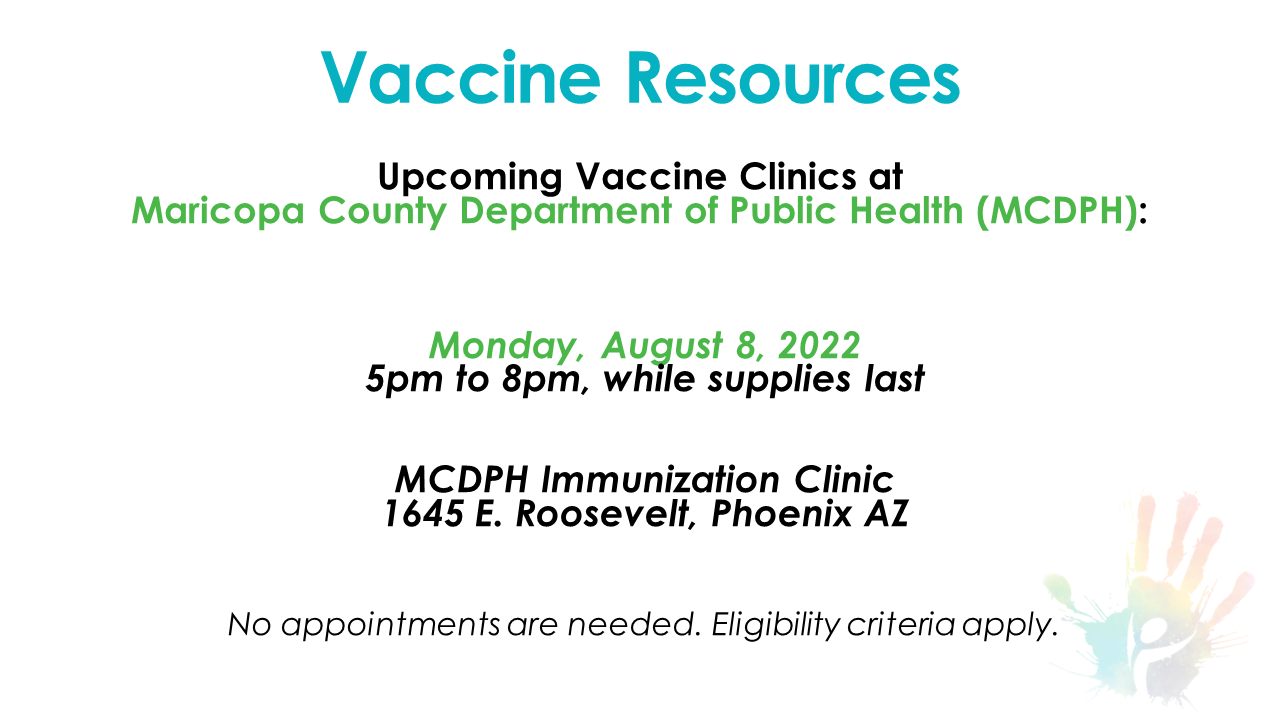
Updated June 2024 - The Southwest Center is no longer providing the mpox vaccine. However, you can still schedule an appointment with the Maricopa County Department of Public Health. Please click here or use the vaccine locator below. If a need arises due to a resurgence, we will reactivate this service.
Vaccination is an important tool in preventing the spread of mpox. Get vaccinated with both doses of the vaccine for the best protection. Mpox is often transmitted through close, sustained physical contact, almost exclusively associated with sexual contact. If you have symptoms of mpox visit a healthcare provider and get tested, even if you have been vaccinated.
Read more about how to prioritize your sexual health!
For more information on mpox, we invite you to visit:
—The Southwest Center Team
Mpox FAQs:
Below is a list of mpox FAQs and answers from the CDC and AZDHS.
What is mpox?
Mpox is part of the same family of viruses as variola virus, the virus that causes smallpox. Mpox symptoms are similar to smallpox symptoms but milder, and mpox is rarely fatal.
How can mpox be prevented?
Get vaccinated for mpox today! You can schedule your vaccination here.
Avoid close, skin-to-skin contact with people who have a rash that looks like mpox.
Avoid contact with objects and materials that a person with mpox has used.
Wash your hands often with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face and after you use the bathroom.
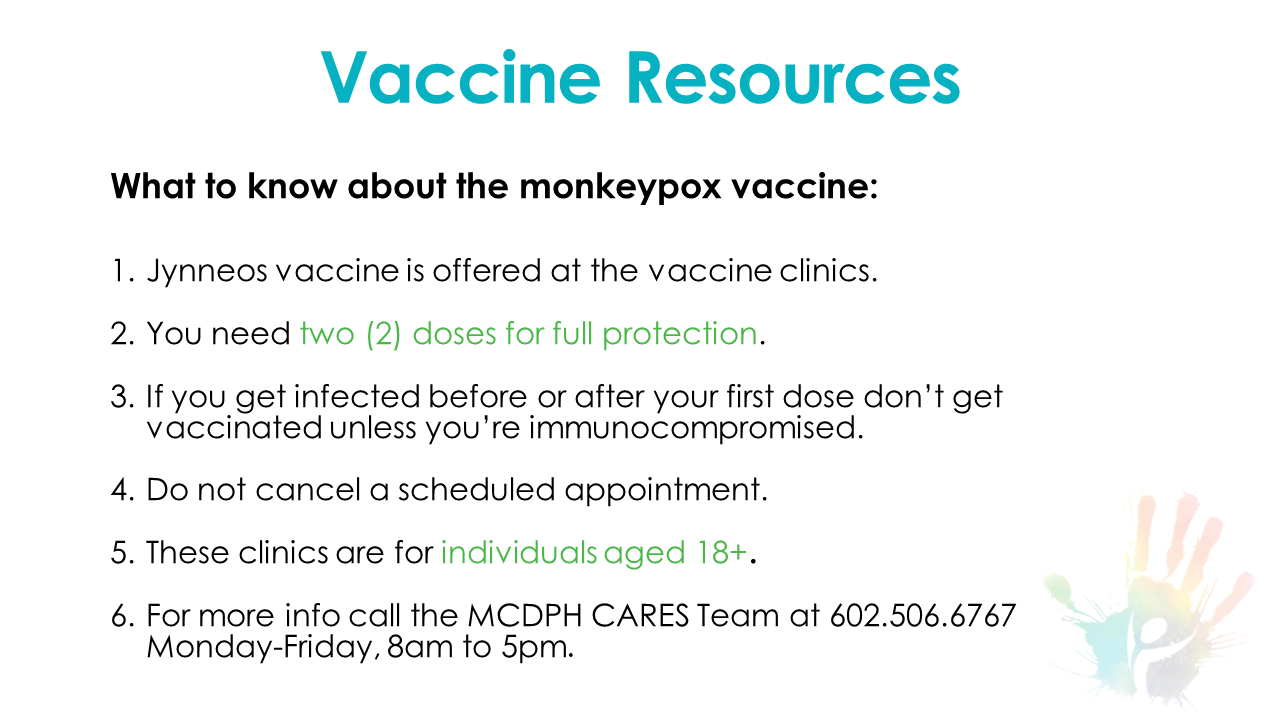
Is there a vaccine to prevent mpox?
Yes! JYNNEOS is a 2-dose vaccine developed to protect against mpox infection. People need to get both doses of the vaccine for the best protection against mpox. The second dose should be given 4 weeks after the first dose.
Where can I get a vaccine for mpox?
For residents of Maricopa County, you can contact the Maricopa Department of Public Health to find local mpox vaccine clinics. Visit their mpox page here, or call MCDPH Cares Team at 602.506.6767.
For residents of Arizona outside of Maricopa County, please contact your county health department.
Who should get vaccinated?
CDC recommends vaccination against mpox for the following people:
Those identified by public health officials as a contact of someone with mpox
Those with a sex partner in the past 2 weeks who was diagnosed with mpox
Known or suspected exposure to someone with mpox
Those with immune suppression who may be exposed to mpox
What treatments are available for mpox?
There is no specific treatment for mpox, but your healthcare provider may prescribe the antiviral tecovirimat (TPOXX) if you are at risk for severe illness or have a weakened immune system. TPOXX is currently free for those in need of this treatment. Most people will recover fully within 2 - 4 weeks without the need for treatment.
We highly recommend receiving the vaccine as there is no specific treatment for mpox at this time.
What are the symptoms of mpox?
Symptoms usually appear within three weeks of exposure. Some people get a rash first, followed by other symptoms. Others only experience a rash. Symptoms of mpox can include:
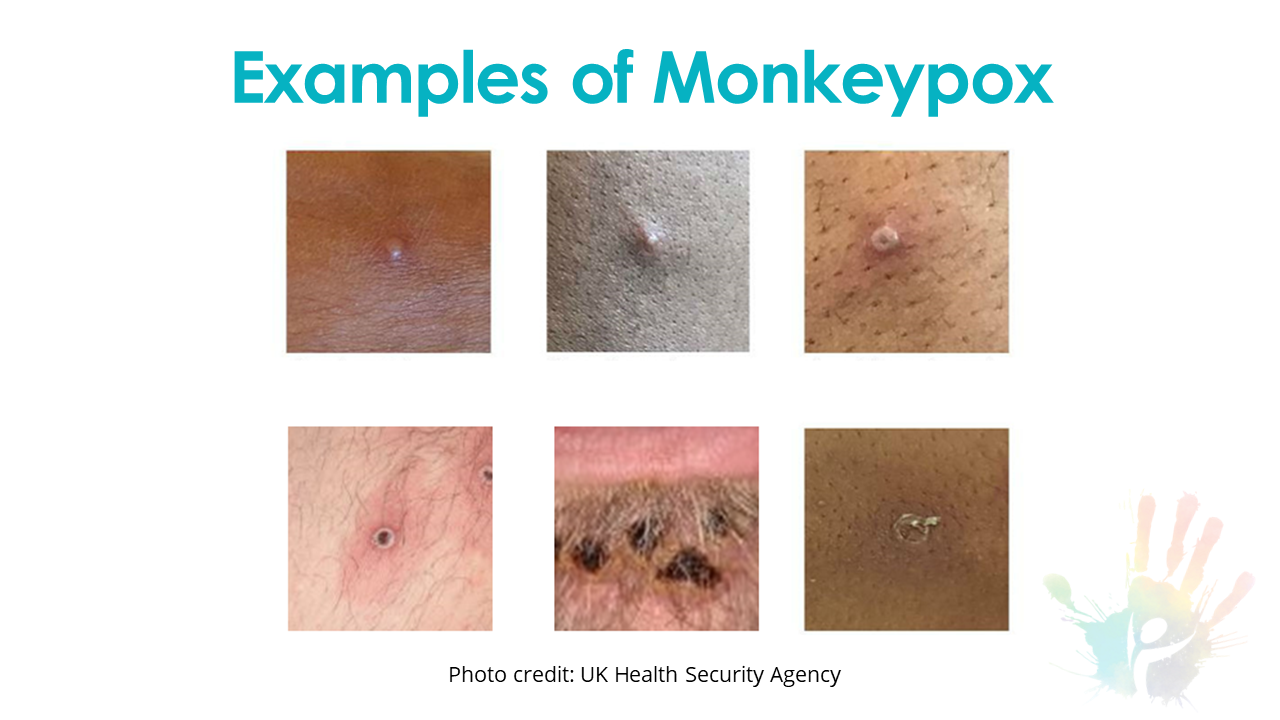
A rash that can look like pimples or blisters that appear on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus.
The rash goes through different stages before healing completely. The illness typically lasts 2-4 weeks.
Swollen lymph nodes (especially in the groin)
Muscle aches and backache
Headache
Fever
Chills
Respiratory symptoms (e.g. sore throat, nasal congestion, or cough)
What should I do if I have symptoms?
See a healthcare provider if you notice a new or unexplained rash or other mpox symptoms.
Remind the healthcare provider that mpox is present in the United States.
Avoid close contact (including intimate physical contact) with others until you see a healthcare provider.
Avoid close contact with pets or other animals until you see a healthcare provider.
If you’re waiting for test results, follow the same precautions.
If your test result is positive, stay isolated and observe other prevention practices until your rash has healed, all scabs have fallen off, and a fresh layer of intact skin has formed.
Remain isolated if you have a fever, sore throat, nasal congestion, or cough. Only go out to see a healthcare provider or for an emergency. Avoid public transportation.
If you must leave isolation, cover the rash and wear a well-fitting mask.
How does mpox spread?
Mpox can spread in a few different ways but often occurs through close skin-to-skin contact with someone infected with mpox.
Direct contact includes:
Skin touching an infected person’s rash, scabs, or bodily fluids.
Touching objects or personal items that have been used by someone with mpox AND not properly disinfected or cleaned.
This includes bedding, towels, fetish gear, and sex toys.
Respiratory large droplet secretions.
Intimate, sexual contact with an infected person including oral, anal, and vaginal sex or touching.
Hugging or kissing a person who has mpox.
Prolonged face-to-face contact with a person who has mpox.
A pregnant person can spread mpox to their fetus through the placenta.
Mpox can also be spread from infected animals, either by being scratched or bitten by the animal, but that has not been the primary mode of transmission for the 2022 outbreak in the U.S.
Is mpox a sexually transmitted infection (STI)?
Mpox can more accurately be described as “sexually transmissible.” In other words, sex is just one of the ways that mpox can be spread.
In the past, mpox outbreaks have been linked to direct exposure to infected animals and animal products, with limited person-to-person spread. In the current mpox outbreak, it is spreading primarily through close personal contact. This may include contact with infectious lesions or respiratory secretions via close, sustained skin-to-skin contact that occurs during sex. However, any close, sustained skin-to-skin contact with someone who has mpox can spread it. The contact does not have to be exclusively intimate or sexual.
Will mpox treatment or vaccine interact with HIV medications?
The CDC recommends people living with HIV receive the mpox vaccine. JYNNEOS is considered the safest mpox vaccine for those living wtih HIV.
Data is limited, but most HIV treatment can be safely given with mpox treatment and smallpox vaccines. People with HIV should inform their healthcare provider of all their medications to help determine if any interactions exist.
Are people living with HIV more likely to have a more severe illness if they get mpox?
CDC continues to monitor mpox among people living with HIV.
The World Health Organization (WHO) mpox guidance states, “People living with HIV on antiretroviral therapy with suppressed viral load are not considered to be immunosuppressed.”
However, people living with HIV who are not virally suppressed may be at increased risk for severe illness and death from mpox.
If I test positive/am diagnosed with mpox, how do I protect my household?
People can spread mpox from the time symptoms start until all symptoms have resolved, including full healing of the rash with the formation of a fresh layer of skin (2 to 4 weeks). Individuals should remain isolated at home and away from others until all symptoms have resolved. People confirmed to have mpox should:
Avoid all close/physical contact, including but not limited to hugging, kissing, touching, and any sexual contact
Avoid sharing or handling objects that other people or animals use
Launder and disinfect items that have been worn or handled and surfaces that have been touched by a lesion
Avoid crowds and congregate settings
Wash hands often with soap and water or use an alcohol-based hand sanitizer, especially after direct contact with the rash
If you are unable to remain fully isolated throughout the illness, you should do the following:
While symptomatic with a fever OR any respiratory symptoms (cough, sore throat, nasal congestion) remain isolated at home and away from others unless it is necessary to see a healthcare provider
While a rash persists but in the absence of a fever or respiratory symptoms:
Cover all parts of the rash with clothing, gloves, and/or bandages
Wear a well-fitting mask around others*
*Masks should fit closely on the face without any gaps along the edges or around the nose and be comfortable when worn properly over the nose and mouth.
Can my pet get mpox?
Mpox is zoonotic, meaning it can spread between animals and people. However, CDC does not currently believe that mpox poses a high risk to pets. We are continuing to monitor the situation closely.
Where can I find more information on mpox?
New information is continuing to develop. Please check the pages below for more detailed and up-to-date information.
Mpox Town Hall Presentation





A Message About Mpox From Our Medical Director, Randy S. Gelow II, MD, AAHIVS
Community at Large,
Having been in a fear-provoking pandemic mindset the past few years and feeling like we finally started making some progress of sorts, I understand the fear when we hear about a “new” infection.
Let me start by giving a little background. Mpox was first identified in the 1950s in Monkeys (hence its name) and in the 1970s in humans and has been endemic in many parts of Africa with occasional small outbreaks outside Africa since its detection. This virus is similar to the eradicated Smallpox virus which was done successfully with the help of vaccination (more on this later). In Africa, mpox has been fatal in 10% of people infected which is quite high. As with any “new” infection, the news tends to sensationalize the story a bit, but in doing so brings awareness that we wouldn’t have otherwise.
Mpox is transmitted via close contact, such as through direct physical contact, exposure to large respiratory droplets (think sneezing, coughing), or through contact with fluids (semen, vaginal, blood, saliva, etc.) from an infected individual to eyes, nose, mouth or through broken skin. Given the time frame from exposure to symptom onset being on average 7-14 days (but can be 5-21 days), you can understand exposures might happen before someone knows they are infected. It’s important to be able to recognize symptoms immediately to help decrease this risk.
Mpox is hallmarked by the same symptoms as many other conditions including fever and chills but also has a special rash that looks similar to blisters (which can present on the body, genitals, anus, and/or hands), and usually always swelling of lymph nodes of neck/armpit/groin areas. Those that have received the smallpox vaccine (which was discontinued in 1972 and often left a “scar” on the arm afterward) do have about 85% protection against mpox due to the similarity of the two. The mpox and smallpox viruses are not related to Chickenpox or Shingles as some might have heard, and infection or vaccination to either of these two are not protective against Mpox or smallpox.
Unlike the initial period after COVID when we did not have treatment, we do have some treatment options for mpox if you are to be infected, but many options would have to be administered in a hospital setting as they are not readily available in pharmacies or primary care offices. Remember that with a 10% fatality rate, we need to make sure we act quickly. There is a vaccine that is available for mpox as well but is not available to the general public, so prevention is key right now.
As with many infections that are transmitted via close contact, the LGBTQ+ community can be unfairly stigmatized. As many may know (and some many not), our community is very close, and over the summer Pride Season, have many larger gatherings which can increase transmission risk and likely is contributing to the higher infections seen among LGBTQ+ members. Ways we can help protect ourselves and others is by making sure we know the symptoms listed above to quickly identify if we might have been exposed, so we are able to see a doctor to be evaluated before we potentially expose other people. In addition, it’s important to remember that decreased direct physical contact and consistent hand washing is helpful to reduce spread.
I know this can bring back fears which many still have but together, we can get through this as we have done with so many other challenges. Please reach out to your primary care provider or a member at Southwest Center for more information. Additional information can also be found on the CDC which routinely updates at https://www.cdc.gov/poxvirus/mpox/index.html.
Randy S. Gelow II, MD, AAHIVS
Medical Director
Southwest Center
1101 N Central Ave, Suite 200 | Phoenix, AZ 85004
